ECON2101 Cost Benefit Analysis Final Case Study – Indigenous Health Clinic Assignment | UQ
| Category | Assignment | Subject | Economics |
|---|---|---|---|
| University | The University of Queensland | Module Title | ECON2101 Cost Benefit Analysis Final Case Study – Indigenous Health Clinic |
ECON2101 Instructions:
This assignment will consist of a group task worth 30% and an individual reflection worth 10%, for a total of 40% of your final grade. The case study can be done individually or as a group of TWO students. Please note that this task is a significant amount of work for an individual, so groups are encouraged.
The assignment must be submitted electronically through the Online Submission links in the Assessment section of the Course Blackboard site.
- Part 1 MUST be submitted as an Excel file (.xls or .xlsx) – only one submission per group is required.
- Part 2 MUST be submitted as a Word file (.doc or docx) – only one submission per group is required.
- Part 3 MUST be submitted as a Word file (.doc or .docx) – each student must submit their own reflective taskfor marking.
Further details to be announced on Blackboard.
Groups must be finalised by 5pm, 6th June. No changes are allowed after this date. Remember that each value should be entered into the spreadsheet only once. Marked out of 80 points (weighted to 40% of your final grade).
Background A regional health authority is considering the development of a community-led Indigenous health clinic in a remote area of Queensland. The clinic would provide culturally safe primary healthcare services, preventative programs, and social and emotional wellbeing support tailored to the needs of Aboriginal and Torres Strait Islander (ATSI) peoples. To assist in evaluating the investment, the authority has asked you to provide a cost-benefit analysis (CBA) to determine the feasibility of the project. As part of this analysis, the authority would like you to examine the potential costs involved in establishing and operating the clinic, as well as the expected benefits to individuals, families, and the wider community. Additionally, the CBA should consider how the proposed clinic aligns with national Closing the Gap targets and regional strategies to improve long-term health outcomes for Indigenous Australians.
The facility is expected to be operational by the start of 2026 and will operate for 20 years. The initial capital investment is scheduled for 2025, with additional purchases required in 2026. In your report to the regional health authority stakeholder, you will need to discuss the results from the Investor, Social, and Disaggregated analyses. You will also need to consider any relevant literature or reports on the evaluation of the external benefits of improved health as part of a program to support the local government and community.
Are You Looking for Answer of ECON2101 Assignment
Order Non Plagiarized Assignment
ECON2101 Part 1- Spreadsheet Group Task – 30 marks (15%)
a) Market and Investor Analysis Development of the new indigenous health clinic requires the preparation of a site and a prefabricated building for the clinic. The custom-designed prefabricated building is built off-site and transported for assembly The cost of the prefabricated building is $1.25 million, but there will also be an expected transportation and set up cost of $150,000.
The regional health authority plans to rent a location for the clinic, however site preparation including basic landscaping, fencing, and 8-10 car parks for staff and patients will be required. This site preparation is expected to cost $150/m² for preparation of 750 m² of the site including the cost of the new car parks.
The clinic will feature three patient consultation rooms, an administrative area, and a dedicated pathology room, designed to support efficient and high-quality healthcare delivery. The medical treatment rooms will be fitted out in 2025 at a cost of $40,000 per room. Furniture for the consultation rooms and administrative area will also be purchased in 2025, with an allocated budget of $55,000. Equipment for the pathology room is scheduled for purchase in 2026, with an expected cost of $45,000. An additional $11,000 has been budgeted for 2026 to cover any unforeseen furniture requirements that may arise as operations expand. Further, the health clinic requires an IT system and software at a cost of $100,000 for recordkeeping, scheduling, and service efficiency. Given the facility is in a regional area, two 4WD or SUVs with regional suitability will be purchased at a cost of $75,000 each. To ensure uninterrupted operations in a remote setting, a reliable backup power source is essential. A diesel generator will be installed at an estimated cost of $40,000, based on current market prices for a high-quality model with a 100-litre fuel tank. This generator is capable of running for 13 hours on a single tank, providing critical support during power outages. To ensure readiness, 1,000 litres of diesel fuel will be procured in 2025 at a cost of $2.20/L to support ongoing use of the vehicles and generator.
The clinic will need to purchase the following items in 2026 as part of the initial investment:
- Medical supplies and pharmaceuticals will be required based on projected patient volumes. With two General Practitioners (GPs), each seeing 25 patients per day for approximately 20 – 24-minute consultations, and working 5 days per week for 48 weeks per year, the total number of annual patient visits has been estimated accordingly to allow for personal leave.
- Costs for medical supplies and pharmaceuticals are calculated on a per patient per year (PPPY) basis, with expected average costs of $110 for medical supplies and $159 for pharmaceutical supplies.
- While point (1) estimates the total number of visits, calculating costs on a per patient per year (PPPY) basis requires adjusting for the average number of GP visits per patient in regional areas, which is currently 3.4 visits per year.
- To ensure readiness, an initial stock of medical and pharmaceutical supplies will be pre- purchased to cover 30% of the expected patient volume calculated in (1). As part of the project, the clinic will need to invest in working capital in 2026to assist in maintenance of the facilities.
The working capital items have been provided in Table 1.
b)Social Analysis You now need to consider the social CBA. Due to taxes, duties, and subsidies we are required to calculate the relevant shadow prices for the following:
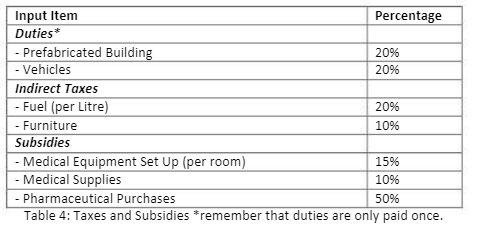
As we observe taxes and subsidies only on inputs in this project, we assume that inputs represent additional quantities supplied (not diverted from other uses). It is also noted that land has an opportunity cost of $0 and the opportunity cost of casual labour is 60% of the market wage for casual workers. All other workers are employed from elsewhere and should be costed at the market wage.
To estimate the external benefits of the new Indigenous health clinic, several key factors have been considered to reflect improvements in access, health outcomes, and community wellbeing
(1)Reduced travel burden
The clinic will significantly reduce the need for long-distance travel to access healthcare. For 50% of total patient visits, travel time to receive healthcare is expected to decrease by 70 minutes. This is particularly valuable in remote and regional Indigenous communities where access to local, culturally safe care is limited.
– The value of time saved from reduced travel is estimated using a market wage rate of $39.70 per hour, which serves as a proxy for opportunity cost.
(2)Fewer potentially preventable hospitalisations
Improved access to timely primary care will reduce avoidable hospital admissions. It is estimated that 15 individuals per year will avoid hospitalisation due to receiving early intervention locally. With an average hospital stay of 4 days at a cost of $3,595 per day, this represents a significant health system saving.
(3)Improved quality of life
The clinic is expected to enhance overall wellbeing, particularly for Indigenous patients through culturally appropriate care. It is estimated that 75 patients per year will experience a 0.025 gain in QALYs (Quality-Adjusted Life Years). Based on a willingness-to-pay value of $28,000 per QALY.
These benefits highlight the broader social value of the clinic beyond direct medical services, particularly in addressing health inequities faced by Indigenous Australians.
Buy Answer of ECON2101 Assignment & Raise Your Grades
Order Non Plagiarized Assignment
ECON2101 Part 2 – Written Report Group Task – 30 marks (15%)
Using your results from Part 1 of the case study, write a comprehensive report analysing the results of your CBA. In your report ensure you:
- Provide professional recommendations to the health authority on whether it should implement the re-development project. You are expected to research relevant literature on indigenous health.
- Outline the approach and results of sections a) to d) in Part 1. In your response you should investigate which variables should be subject to a partial sensitivity analysis in addition to the results of d).
- Identify considerations for your analysis or any alternative approaches that would improve on the current format of the CBA.
Word limit: 1500 words
ECON2101 Part 3 – Reflective Assessment Individual Task – 20 marks (10%)
Critically reflect on the CBA task from the Case Study. In your answer,
- determine and establish the relevance and authenticity of the case study task as part of your development in a professional context.
- reflect on your individual challenges or challenges faced as part of a group.
Word limit 750 words.
